Article: Foo LL et al.
Myopia or short-sighted-ness is a common problem in Singapore. It typically starts at childhood, increases till the mid-late teens, with increased eyeball growth, before stabilizing. Singapore’s unique physical and socioeconomic landscape has contributed to some of the highest levels of myopic prevalence seen globally. At present, approximately 20% of Singaporean children are myopic by the age of 7, with the prevalence exceeding 70-80% upon completion of tertiary education. Some 15-20% of young adults in Singapore will become highly myopic (i.e. have myopia more than 6.00D).
In high myopia, the eyeball has grown much larger than it should be, and this leads to increased structural strain on structures within the eye. High myopia carries an increased risk of sight-threatening complications such as retinal detachment, open-angle glaucoma, myopic macular degeneration and choroidal neovascularization (CNV) [1, 2]. Occurrence of these complications would inevitably increase public health burden [3], and lead to loss of productivity [4].
If we could predict which children are ‘at risk’ of developing high myopia with precision, we may be able to institute appropriate myopia control interventions early and slow the development of myopia. These interventions include atropine eye drops and optical devices (e.g., myopia control spectacles and contact lenses).
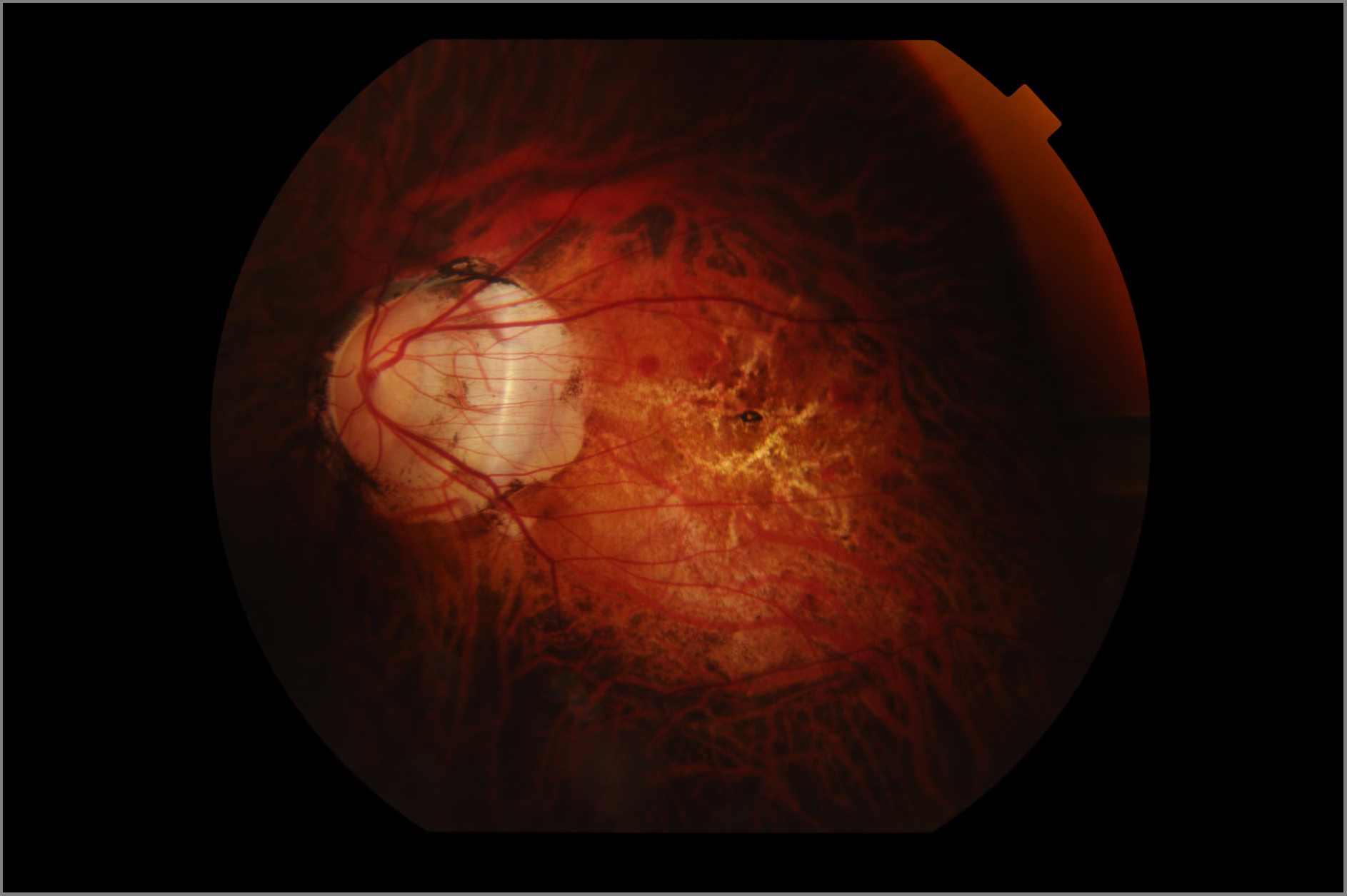
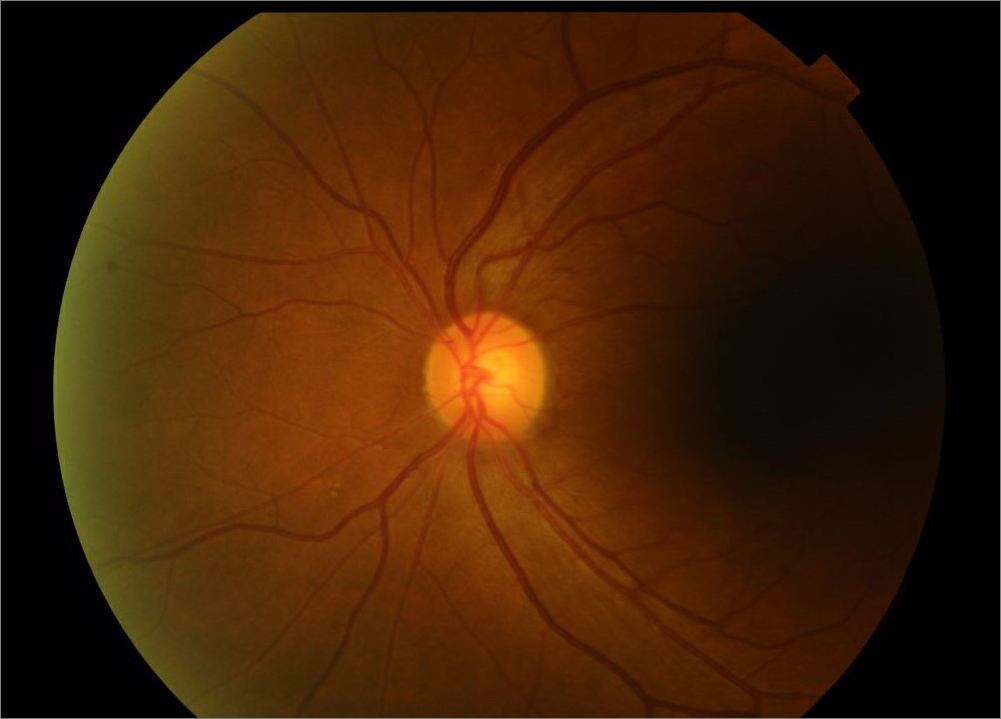
Figure 1: Fundus image of a patient with high myopia and its associated degenerative changes including tilted disc, peripapillary atrophy, myopic macular degeneration, and lacquer cracks (left) compared to a normal fundus image (right)
Using artificial intelligence (AI), we developed algorithms to predict the 5-year development of high myopia in a multi-ethnic group of schoolchildren aged between 6 to 12 years old. Our algorithms demonstrated clinically acceptable predictive performance ranging from 90-98% in future high myopia prediction. Importantly, simply with just a fundus image alone, we were able to achieve a performance of 94%. Moreover, our models appropriately identified the disc and macular as areas of interest, consistent with areas of future myopic disc changes and myopic macular degeneration.
Figure 2: Fundus imaging showing the areas of interest identified by the artificial intelligence: disc (left) and macular (right)
Our AI algorithms have the potential to be translated and implemented into community or school-based programs via integration into fundus camera to identify at-risk children for further assessment and intervention if required. With future development of this AI system with involvement of children of different ethnicity and geographical location, it has the potential to be used as a clinical assistive tool to risk stratify children who are at higher risk of developing high myopia. Through early identification, targeted and timely myopia control therapies may be instituted to reduce the risk of developing high myopia in these children.
- Wong TY, Ferreira A, Hughes R, Carter G, Mitchell P: Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. American Journal of Ophthalmology 2014, 157(1):9-25 e12.
- Ikuno Y: Overview of the Complications of High Myopia. Retina 2017, 37(12):2347-2351.
- Morgan IG, Ohno-Matsui K, Saw SM: Myopia. Lancet 2012, 379(9827):1739-1748.
- Naidoo KS, Fricke TR, Frick KD, Jong M, Naduvilath TJ, Resnikoff S, Sankaridurg P: Potential Lost Productivity Resulting from the Global Burden of Myopia: Systematic Review, Meta-analysis, and Modeling. Ophthalmology 2019, 126(3):338-346.
Contributed by:

Dr Foo Li Lian
Consultant, Myopia Service
Cataract & Comprehensive Ophthalmology Department
Singapore National Eye Centre
Back to
EyeSight main page.
