Ms Ng Lai Heong is an Assistant Nurse Clinician at the Singapore National Eye Centre (SNEC) Operating Theatre and the nursing team lead for our Ocular Brachytherapy service.
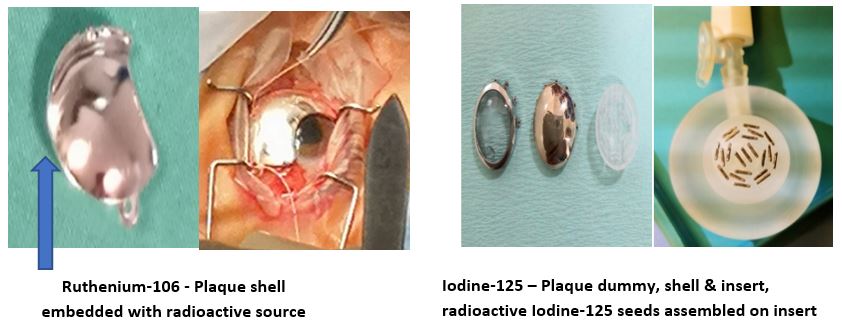
Brachytherapy is a service introduced in 2018. It involves the use of low-dose radiation to help control cancerous cell growths within the eye. This involves the application of radioactive plaques (made either of Iodine-125 or Ruthenium-106) onto the eye surface (episcleral) to treat tumours such as ocular melanoma, choroidal hemangioma, retinal angioma; vasoproliferative tumours & retinoblastoma. Previously, patients with ocular tumors would have to seek treatment overseas, or to have their eyes removed. With this new service, 90% of the patients in Singapore are now able to have this globe-sparring therapy locally.
The service includes a collaboration between SNEC and National Cancer Centre (NCCS) Radiation Oncology department, and was formed by A/Prof Gavin Tan, Senior Consultant, Surgical Retina Department, SNEC. The team (including doctors and nurses) visited Hospital Clinico Universitario, Valladolid, Spain, in 2018 for 4 days (duration) to be trained in this treatment.

SNEC & NCCS
team training in Hospital Clinico Universitario, Valladolid, Spain
Q: Hi Lai Heong, what are the roles and responsibilities of a brachytherapy nurse?
In setting up the service, I worked closely with A/Prof Gavin Tan in ensuring policies and protocols are in place, creating the reference file, planning the workflow and developing pictorial guide to help train our OT staff. Working with radioactive substances hold exposure risk to staff and patients, and we needed to ensure that all radiation safety protocols were in place.
Being in-charge, I need to maintain close communication between all the relevant stakeholders. When a case is listed, I note the surgery date for insertion and removal procedure, what type of radioactive implant is required, and ensure that it is procured and delivered. Then we need to see to the sterilization of items, and prepare the theatre for surgery, and ensure all parties are appropriately informed. I need to ensure all protocols are adhered to, especially during handling, insertion, removal and disposal of the radioactive items.
I am also involved in training and education, and conducting in-service training to educate nurses on the pre-, intra- and post-operative care for the patients.
There must be lots of preparation that goes on for each case!
Yes. Everything needs to be planned so that things go like clock-work. Many processes need to be activated once a case is listed. We need good communication between all parties to ensure everything goes smoothly.
Pre-operatively, we need to:
- Ensure availability of type and size of implant for the patient
- Prepare instruments and consumables required for the surgery
- Sterilize and assembly of radioactive implant with the NCCS Radiation Oncologist and Medical Physicist
- Ensure proper safekeeping of the implant in NCCS as per protocol
- Plan for surgical team and inform them of the potential contraindications of radioactive implants. (e.g. no pregnant staff)
- Ensure proper pre-operative patient education on eye care and eye drops instillation are conducted by day surgery / outpatient clinic staff
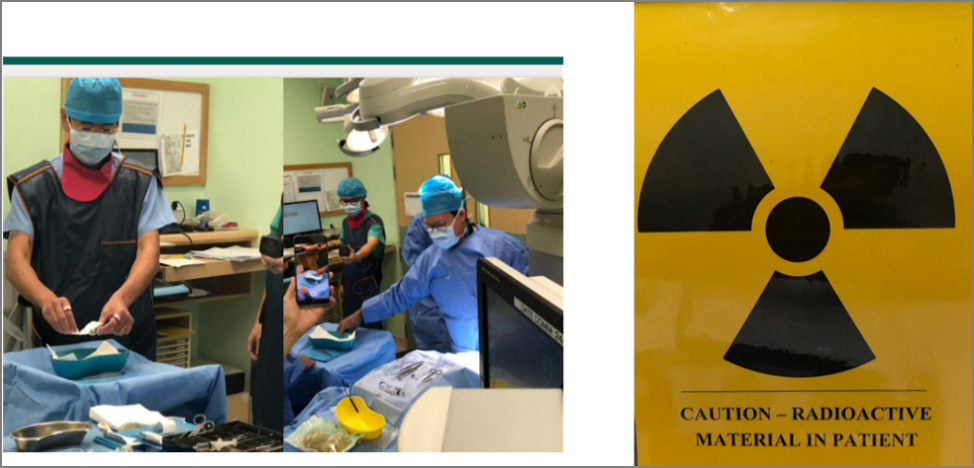
Intra-operatively, we need to emphasize radioactive safety:
-
Ensure that preventive measures for radiation is in placed
-
Make sure each staff have their personal dosimeters in working condition
-
Ensure that surgical team don lead thyroid shield, lead apron and personal dosimeter tag at all time and adhere to all radioaction safety measures
Post-operatively, we need to:
- Ensure post-operative clinic review is done in an isolated room, and that any at risk persons (e.g. pregnant staff) are warned to avoid the area.
- Ensure the team of staff caring for the patient adheres to the radiation safety protocol
- Plan for removal of implant in 5-7 days, depending on treatment duration planned by NCCS Medical Physicist and Radiation Oncologist
Who are the team members involved?
From the start of the patient journey in the SNEC Outpatient Department (OPD), the Operation Theatre (OT) and then the Day Ward (DW), each department assigns 2 staff as point of contact for seamless communication.
The NCCS team handles the radioactive source on arrival and storage. Sterilization of implant are done collectively between NCCS and SNEC Theatre Sterile Supply Unit (TSSU) team.
We had a Brachy-team and department chat group in place to ensure everyone know what is happening each step along the way.
What are your plans for the future?
Since we started our service, we have done 14 cases. We continue to train and groom new staff; and work on our work-flow and protocol. Currently I work closely with Senior Staff Nurse Sam Mei Poh and Eng Sze Yin to train them as future team lead.
Moving forward, we hope that this service will be more established in Singapore and be able to provide better medical care for the patients even on the international platform. With this, it is important to continuously keep ourselves updated with the latest medical technological advances and educate the next generation of nurses.

New Brachy team leader SSN Sam Mei Poh leading the team for the 14th case done recently
Contributed by:

Ng Lai Heong
Assistant Nurse Clinician
Operating Theatre
Singapore National Eye Centre
Back to
EyeSight main page.
